ROCHESTER, Minn. — Opioids have long been discredited for the care of most chronic pain, and a growing body of research has even begun to cast doubt on their usefulness following common surgeries.
With the case for opioids in medicine having largely collapsed, a new book asks what lies ahead for the future of non-opioid pain management. It's a question of what might have been, says the author, had pain medicine not been hijacked by the lies that gave rise to a deadly opioid epidemic in the first place.
ADVERTISEMENT
"I think one of the things that's happened because of the opioid epidemic is the issue of chronic pain has now become something that we cannot ignore," says , a physician with the Harvard Medical �������� and author of
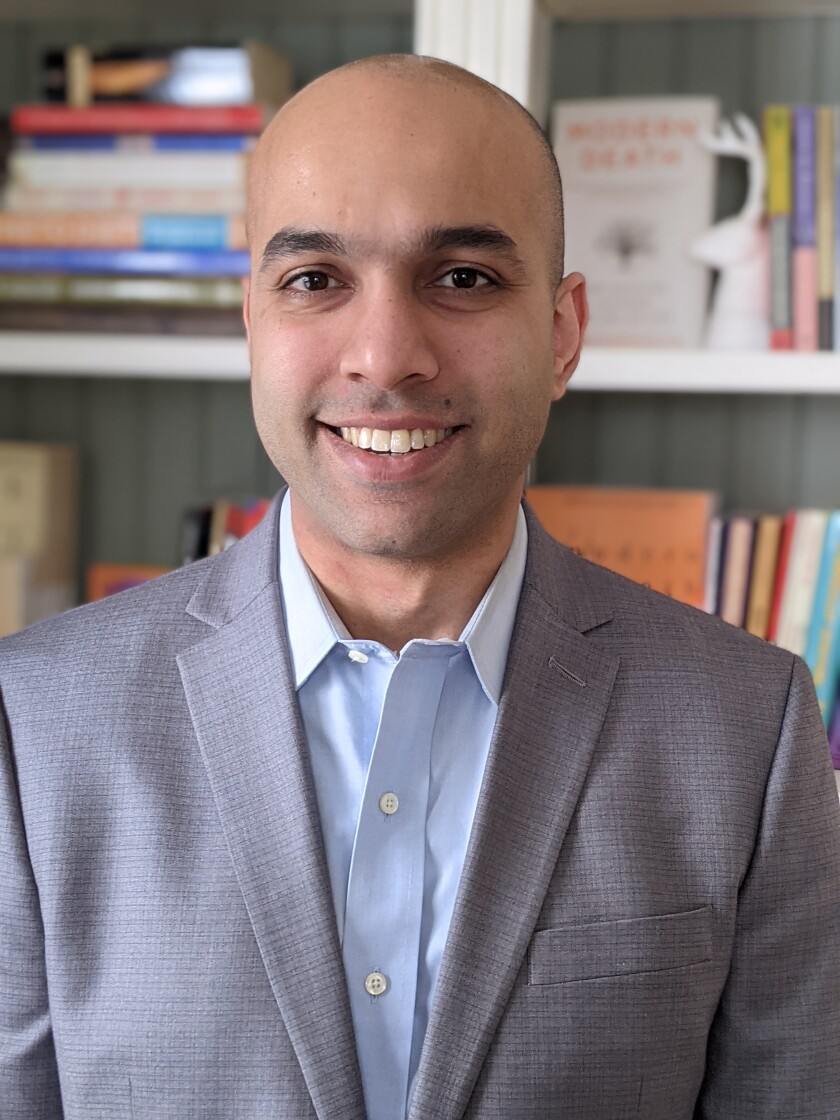
A writer for The New Yorker who has battled chronic pain since a horrific weightlifting accident as a medical student, Warraich describes the utility of an integrated, multi-disciplinary approach to the care of chronic pain.
It's a post-opioid road map that trades what he describes as a dangerous, uniquely American expectation of a pain-free life, for one of pain without suffering — of "living well despite the pain."
"Part of why we ended up in this situation is that we tried to simplify pain, which is one of the most complex things that a human being can experience, and to essentially say that it's a vital sign like heart rate or blood pressure," Warraich said during an interview with Forum News Service.
To the contrary, Warraich argues, pain sensitivity is an inherently subjective, context-dependent experience. He points out that a runner's bodily aches will mean something vastly different the minute after crossing the finish line.
In this view, chronic pain is less of a wound that has not healed — a prolonging of acute pain — than a malfunctioning convergence of individual beliefs and feelings, as well as an over-sensitivity to bodily signals, a defense mechanism that becomes its own kind of cage.
It all adds up to a subjective phenomenon for which few doctors trained to read blood panels or consult MRI images are prepared to treat.
ADVERTISEMENT
"When someone's coming in with abdominal pain that's brand new, you want to get to the bottom of what's causing that pain," Warraich says of the doctor's conundrum. "But for patients with chronic pain, most of the time there's no new process."
"In that situation, it's really about understanding what place pain holds in their life — what it means to them, and how it's affecting their lives. That's not something we're trained to do."
Two systems of pain
"The Song of Our Scars" intersperses the sociology, psychology and science of pain, with the long, tragic story of opioids in human history and Warraich's own journey through suffering to regain his function.
A self-described member of "the opioid generation" of doctors who trained under the falsehoods that gave rise to the opioid epidemic, Warraich rejected opioids for his own injury due to a medical environment in which "we were overwhelmed with patients suffering the adverse effects" of the drugs.
The Centers for Disease Control and Prevention for long-term use since 2016, while Mayo Clinic now "a last resort" only, limited to pain caused by cancer or its treatment. Less expected has been the fall from favor of even a standard short-course prescription for post-operative pain, according to .
Addiction and overdose are the attention-grabbing adverse effects of opioids, not to mention lesser risks such as constipation, obesity, impotence and low testosterone. But some of the book's most memorable passages are those in which Warraich describes the negative effects of opioids on the human endogenous opioid system.
The body makes its own opioids, and they help us to cope with stress. By blunting this system, Warraich says, prescription opioids can worsen our very vulnerability to pain, stress and depression — even harming our ability to enjoy small pleasures or feel connection to others.
ADVERTISEMENT
Warraich rejected surgery for his back condition upon heeding the advice of a surgeon who said that a spine which has been operated on "is never the same."
While the book examines the pros and cons of a host of alternative pain control methods that remained — including hypnosis, ketamine and cannabis — its focus settles around cognitive and physical therapy, and addressing the so-called "pain behaviors" people with chronic pain often deploy out of self-protection.
Among the avoidance and attentional strategies that can prolong pain, Warraich singles out the need to push past pain-promoting cognitions such as "catastrophizing," as well as "kinesophobia," a word for the fear of movement.
It's a non-opioid model of care that, while not as readily authorized by payers as drugs or surgery, has increasingly become the standard in Pain Medicine & Rehabilitation at reputable medical centers.
"I think we have created a culture in which we look to medical intervention for relief," he said. "Sometimes that's good, but I think for pain, the more you try to control pain, the more it actually controls you back."
"Which is why I think finding a way to coexist with pain can not only help us live our lives better, but actually reduce the intensity of the pain as well."









